Medical Disclaimer
The information presented in this article is for educational purposes only and should not be considered medical advice. While there is growing evidence linking gut health and anxiety, this information is not intended to diagnose, treat, cure, or prevent any disease. Always consult with a qualified healthcare professional before making any changes to your diet, lifestyle, or treatment plan, especially if you have pre-existing health conditions or are taking medications.
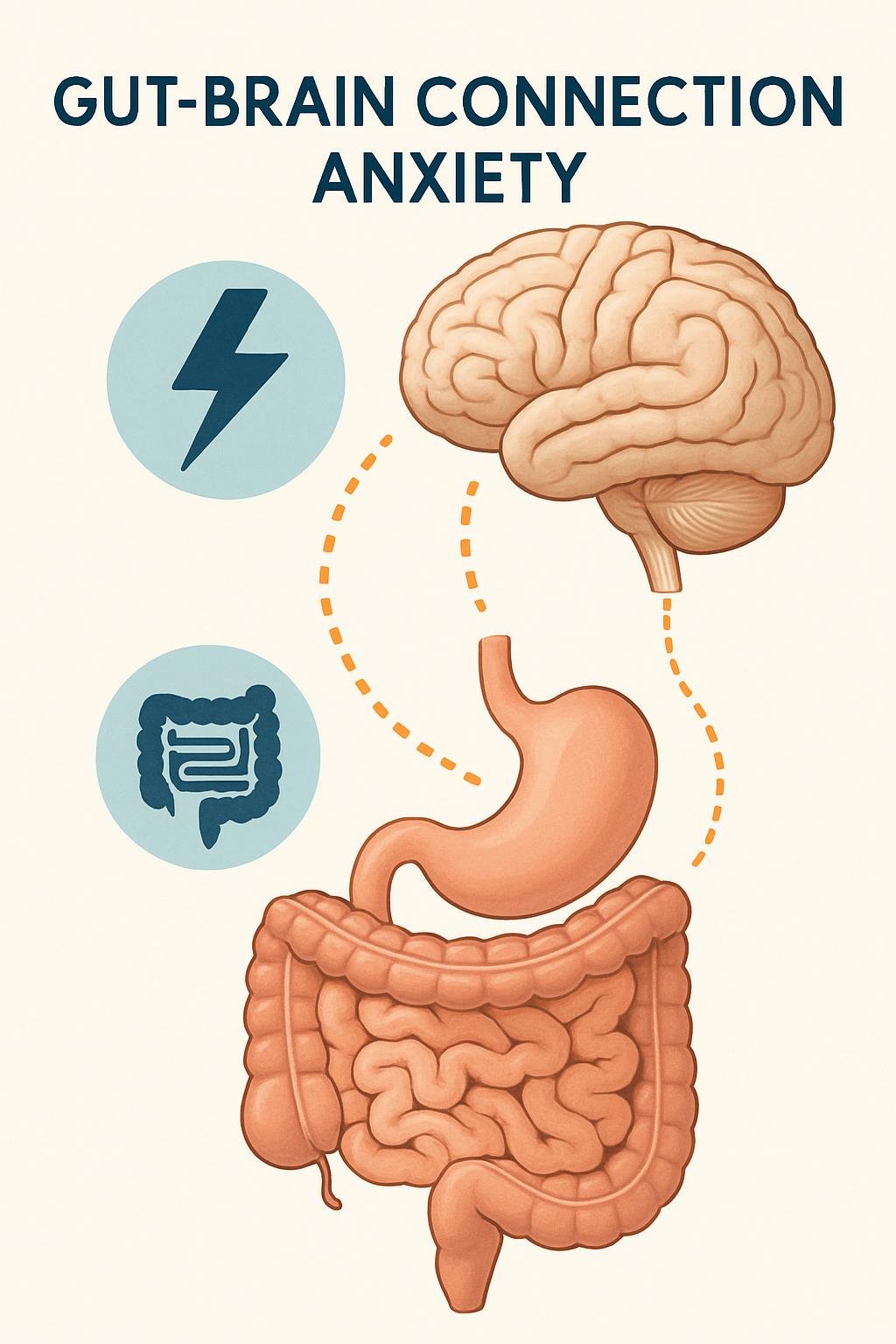
The idea that our gut feelings might be more than just intuition is gaining significant scientific traction. Emerging research is revealing a profound and complex connection between the health of our digestive system—specifically the trillions of microorganisms residing within it—and our mental well-being, including anxiety levels. This intricate communication network, known as the gut-brain axis, suggests that what happens in your gut doesn't just stay in your gut; it can directly influence your mood, stress response, and susceptibility to anxiety.
This comprehensive guide delves into the fascinating science behind the gut-brain connection, explores how imbalances in the gut microbiome can contribute to anxiety, and provides evidence-based natural strategies to support gut health for improved mental wellness.
Understanding the Gut-Brain Axis
The gut-brain axis is a bidirectional communication system linking the central nervous system (brain and spinal cord) with the enteric nervous system (the complex network of nerves within the gastrointestinal tract). This communication occurs through several pathways:
- The Vagus Nerve: This long cranial nerve acts as a direct information highway, transmitting signals between the gut and the brain.
- Neurotransmitters: The gut produces a significant portion of the body's neurotransmitters, including serotonin (often called the "feel-good" chemical) and GABA (an inhibitory neurotransmitter that promotes calmness). Gut microbes play a crucial role in synthesizing and regulating these chemicals.
- The Immune System: The gut houses approximately 70% of the body's immune cells. Gut microbes interact with these immune cells, influencing systemic inflammation, which has been linked to anxiety and depression.
- Hormonal Pathways: The gut influences the hypothalamic-pituitary-adrenal (HPA) axis, the body's central stress response system. Gut microbes can modulate the production of stress hormones like cortisol.
- Microbial Metabolites: Gut bacteria produce various metabolites, such as short-chain fatty acids (SCFAs), which can cross the blood-brain barrier and influence brain function and mood.
This complex interplay means that signals from the brain (like stress) can affect gut function, and signals from the gut (like inflammation or microbial imbalances) can impact brain function and emotional states.
The Gut Microbiome: Your Inner Ecosystem
The gut microbiome refers to the vast community of microorganisms—bacteria, viruses, fungi, and archaea—that live primarily in the large intestine. A healthy adult gut typically harbors trillions of these microbes, collectively weighing several pounds.
Key Roles of the Gut Microbiome
These microbes are far from passive passengers; they perform essential functions:
- Digestion: Breaking down complex carbohydrates and fibers that our bodies cannot digest alone.
- Nutrient Synthesis: Producing essential vitamins like vitamin K and certain B vitamins.
- Immune System Development and Regulation: Training the immune system to distinguish between harmful pathogens and harmless substances.
- Gut Barrier Integrity: Maintaining the intestinal lining, preventing "leaky gut" (intestinal permeability).
- Neurotransmitter Production: Synthesizing or influencing the production of neurotransmitters that affect mood and anxiety.
- Inflammation Regulation: Balancing pro-inflammatory and anti-inflammatory responses throughout the body.
Dysbiosis: When the Gut Ecosystem Is Disrupted
Dysbiosis refers to an imbalance in the gut microbiome—either a reduction in beneficial bacteria, an overgrowth of potentially harmful microbes, or a loss of microbial diversity. Several factors can contribute to dysbiosis:
- Antibiotic use (especially repeated or prolonged courses)
- Poor dietary patterns (high in processed foods, sugar, and low in fiber)
- Chronic stress
- Lack of physical activity
- Environmental toxins
- Certain medications (beyond antibiotics)
- Sleep disturbances
Research increasingly suggests that dysbiosis may contribute to various health issues, including anxiety disorders.
The Gut-Anxiety Connection: What the Research Shows
The relationship between gut health and anxiety is supported by a growing body of scientific evidence:
Animal Studies
Some of the most compelling evidence comes from animal research:
- Studies with germ-free mice (raised without any gut microbes) show exaggerated stress responses and anxiety-like behaviors compared to mice with normal gut microbiomes.
- Transferring gut bacteria from anxious mice to germ-free mice can induce anxiety-like behaviors in the recipients.
- Administering specific probiotic strains to rodents has been shown to reduce anxiety-like behaviors and normalize stress hormone levels.
Human Studies
While human research is still evolving, several important findings have emerged:
- People with certain anxiety disorders show different gut microbiome compositions compared to healthy controls.
- A systematic review published in General Psychiatry found that regulating intestinal microbiota (through probiotics, prebiotics, or dietary changes) may have a positive effect on anxiety symptoms.
- Clinical trials have demonstrated that certain probiotic strains can reduce anxiety scores in both healthy individuals and those with clinical anxiety.
- Patients with irritable bowel syndrome (IBS) and other gastrointestinal disorders have higher rates of anxiety, suggesting a bidirectional relationship.
Mechanisms Linking Gut Health to Anxiety
Several pathways may explain how gut health influences anxiety:
- Inflammation: Dysbiosis can lead to increased intestinal permeability ("leaky gut"), allowing bacterial components to enter the bloodstream and trigger systemic inflammation. Inflammatory markers have been consistently linked to anxiety disorders.
- Neurotransmitter Production: The gut microbiome influences the production of neurotransmitters like serotonin (approximately 90% of which is produced in the gut), GABA, and dopamine—all of which play crucial roles in mood regulation and anxiety.
- HPA Axis Regulation: Gut microbes help regulate the body's stress response system. Dysbiosis can lead to HPA axis dysfunction and abnormal cortisol patterns associated with anxiety.
- Vagus Nerve Signaling: Certain gut bacteria can stimulate the vagus nerve, affecting brain regions involved in anxiety processing.
- Tryptophan Metabolism: Gut microbes influence the metabolism of tryptophan, the precursor to serotonin, potentially affecting serotonin availability in the brain.
Natural Strategies to Support Gut Health for Anxiety Relief
Based on current research, several approaches may help improve gut health and potentially reduce anxiety:
Dietary Approaches
Increase Dietary Fiber
Fiber serves as food for beneficial gut bacteria, helping them thrive and produce beneficial compounds like short-chain fatty acids. Aim for diverse fiber sources:
- Vegetables: Especially leafy greens, Brussels sprouts, broccoli, and artichokes
- Fruits: Particularly berries, apples, and pears with their skins
- Legumes: Beans, lentils, and chickpeas
- Whole grains: Oats, quinoa, brown rice, and barley
- Nuts and seeds: Flaxseeds, chia seeds, almonds, and walnuts
Incorporate Fermented Foods
Fermented foods contain live beneficial bacteria that may contribute to a healthier gut microbiome:
- Yogurt with live active cultures
- Kefir (dairy or water-based)
- Sauerkraut (unpasteurized)
- Kimchi
- Miso
- Tempeh
- Kombucha
Consume Prebiotic-Rich Foods
Prebiotics are specific types of fiber that selectively feed beneficial gut bacteria:
- Garlic and onions
- Leeks
- Asparagus
- Bananas (especially slightly underripe)
- Jerusalem artichokes
- Chicory root
- Dandelion greens
Consider a Mediterranean-Style Diet
Research suggests that a Mediterranean dietary pattern—rich in vegetables, fruits, whole grains, fish, olive oil, and nuts—supports a healthy gut microbiome and is associated with lower rates of anxiety and depression.
Limit Gut-Disrupting Foods
Certain foods may negatively impact gut health:
- Highly processed foods
- Artificial sweeteners
- Excessive alcohol
- Foods high in added sugars
- Emulsifiers (common in processed foods)
Probiotic Supplementation
Probiotics are live beneficial microorganisms that, when administered in adequate amounts, confer a health benefit. Some strains have shown promise for anxiety reduction:
- Lactobacillus rhamnosus: Has demonstrated anxiety-reducing effects in both animal and human studies.
- Bifidobacterium longum: Research suggests it may help reduce anxiety and improve coping with stress.
- Lactobacillus acidophilus: Some studies indicate it may help reduce anxiety symptoms.
- Bifidobacterium bifidum: Has shown potential benefits for stress-related symptoms.
When considering probiotic supplements:
- Look for products with multiple strains
- Check for adequate colony-forming units (CFUs), typically 1-10 billion per serving
- Ensure the product has proper storage requirements and a viable shelf life
- Consult with a healthcare provider, especially if you have existing health conditions
Lifestyle Factors for Gut Health
Stress Management
Chronic stress negatively impacts gut health, creating a vicious cycle that can worsen anxiety. Effective stress-reduction techniques include:
- Mindfulness meditation
- Deep breathing exercises
- Yoga
- Progressive muscle relaxation
- Time in nature
- Regular enjoyable activities
Regular Physical Activity
Exercise benefits gut health by:
- Increasing microbial diversity
- Enhancing gut transit time
- Reducing inflammation
- Improving mood directly through endorphin release
Aim for at least 150 minutes of moderate-intensity activity per week, with a mix of aerobic exercise and strength training.
Adequate Sleep
Poor sleep quality and disrupted circadian rhythms can negatively affect gut microbiome composition. Prioritize sleep hygiene:
- Maintain consistent sleep-wake times
- Create a restful sleep environment
- Limit screen time before bed
- Avoid large meals and caffeine close to bedtime
Mindful Antibiotic Use
While antibiotics are sometimes necessary, they can disrupt gut microbiome balance:
- Only use antibiotics when prescribed and necessary
- Complete the full prescribed course
- Consider probiotic supplementation during and after antibiotic treatment (separated by at least 2 hours)
- Focus on gut-supporting foods after antibiotic courses
Addressing Intestinal Permeability ("Leaky Gut")
Increased intestinal permeability may contribute to the gut-anxiety connection. Some approaches that may help support gut barrier function include:
- L-glutamine: An amino acid that serves as fuel for intestinal cells and may help repair the gut lining.
- Zinc: Plays a role in maintaining tight junction proteins that control gut barrier integrity.
- Collagen peptides: Provide building blocks for repairing the intestinal lining.
- Bone broth: Contains collagen, glutamine, and other compounds that may support gut healing.
- Anti-inflammatory herbs: Turmeric, ginger, and slippery elm may help reduce gut inflammation.
Integrating Gut Health into a Comprehensive Anxiety Management Plan
While improving gut health may help reduce anxiety symptoms, it's most effective as part of a holistic approach:
Complementary Approaches
- Cognitive-behavioral therapy (CBT): Evidence-based psychological treatment for anxiety disorders.
- Mindfulness-based interventions: Can reduce anxiety while potentially benefiting gut health.
- Regular physical activity: Benefits both mental health and gut microbiome composition.
- Social connection: Strong social support is associated with better mental health outcomes.
- Adequate sleep: Essential for both gut health and anxiety management.
When to Seek Professional Help
Consider consulting healthcare providers if:
- Anxiety significantly impacts your daily functioning
- You experience persistent digestive symptoms alongside anxiety
- Self-help measures don't provide adequate relief
- You're considering significant dietary changes or supplement regimens
Working with both mental health professionals and practitioners knowledgeable about gut health (like integrative physicians, functional medicine practitioners, or registered dietitians with specialized training) may provide the most comprehensive approach.
Conclusion: The Future of Gut-Brain Research
The connection between gut health and anxiety represents an exciting frontier in mental health research. While we still have much to learn, the emerging evidence suggests that nurturing our gut microbiome may be a valuable component of anxiety management.
As research continues to evolve, we're likely to gain more specific insights into which microbial strains, dietary patterns, and lifestyle factors most effectively support both gut and mental health. This growing field of "psychobiotics"—interventions targeting the microbiome to benefit mental health—holds promise for more personalized approaches to anxiety management in the future.
In the meantime, the strategies outlined in this article represent evidence-based approaches that support overall well-being while potentially helping to manage anxiety through the gut-brain connection. By nurturing the complex ecosystem within us, we may find new pathways to greater calm and emotional resilience.
References
- Cryan JF, O'Riordan KJ, Cowan CSM, et al. The Microbiota-Gut-Brain Axis. Physiol Rev. 2019;99(4):1877-2013.
- Foster JA, Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36(5):305-312.
- Liu RT, Walsh RFL, Sheehan AE. Prebiotics and probiotics for depression and anxiety: A systematic review and meta-analysis of controlled clinical trials. Neurosci Biobehav Rev. 2019;102:13-23.
- Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017;7(4):987.
- Dinan TG, Cryan JF. The Microbiome-Gut-Brain Axis in Health and Disease. Gastroenterol Clin North Am. 2017;46(1):77-89.
- Bravo JA, Forsythe P, Chew MV, et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci U S A. 2011;108(38):16050-16055.
- Messaoudi M, Lalonde R, Violle N, et al. Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br J Nutr. 2011;105(5):755-764.
- Pinto-Sanchez MI, Hall GB, Ghajar K, et al. Probiotic Bifidobacterium longum NCC3001 Reduces Depression Scores and Alters Brain Activity: A Pilot Study in Patients With Irritable Bowel Syndrome. Gastroenterology. 2017;153(2):448-459.e8.
- Lach G, Schellekens H, Dinan TG, Cryan JF. Anxiety, Depression, and the Microbiome: A Role for Gut Peptides. Neurotherapeutics. 2018;15(1):36-59.
- Fung TC, Olson CA, Hsiao EY. Interactions between the microbiota, immune and nervous systems in health and disease. Nat Neurosci. 2017;20(2):145-155.